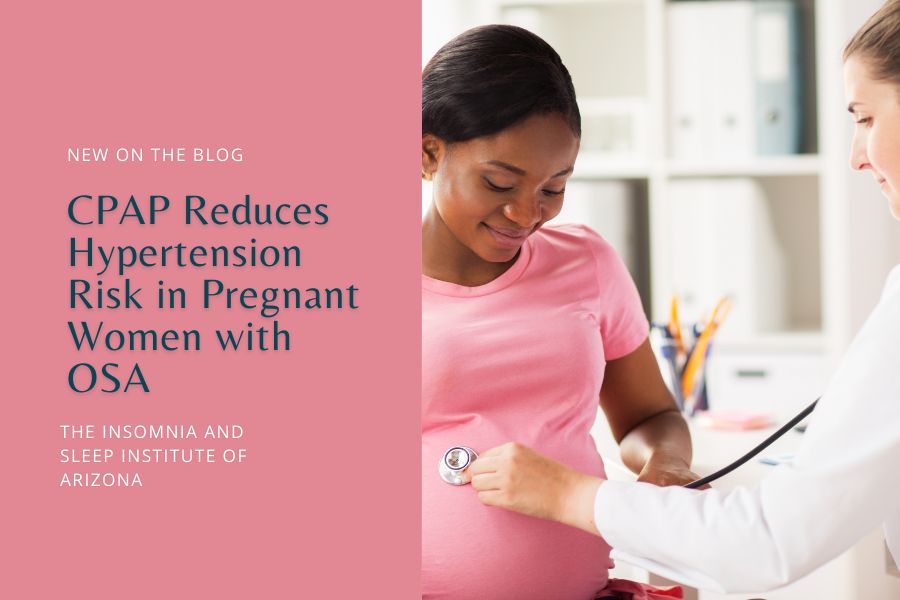
Pregnancy brings many changes. For women with obstructive sleep apnea (OSA), it can also bring increased health risks, including gestational hypertension and preeclampsia.
However, recent research shows a promising solution: CPAP (Continuous Positive Airway Pressure) therapy. It may help stabilize breathing and blood pressure during sleep. CPAP may also significantly reduce the risk of these serious pregnancy complications, supporting both maternal and fetal health.

What Is Obstructive Sleep Apnea (OSA) and How Does It Affect Pregnant Women?
Obstructive sleep apnea (OSA) is a sleep disorder where breathing repeatedly stops and starts throughout the night. The cause is a physical blockage in the upper airway — often from the collapse of soft tissues in the throat. When this happens, airflow is interrupted, causing oxygen levels to drop and forcing the body to wake up briefly to resume breathing. This can happen dozens or even hundreds of times a night, affecting sleep quality and health.
In the general population, OSA is common (around 3-7% of adults). Yet, during pregnancy, the prevalence of OSA is even higher. Particularly in women who are overweight, have a history of snoring, or have pre-existing conditions like hypertension.
It can be worsened due to hormonal changes, increased weight, and fluid retention during pregnancy. OSA during this time is more likely to be more severe. What’s more, pregnant women may experience some form of sleep apnea during their third trimester.
How Does OSA Impact Pregnant Women?
OSA can make pregnant women feel fatigued, irritable, and unfocused. But aside from poor sleep quality, OSA can have serious implications for both maternal and fetal health. Repeated drops in oxygen levels and sleep fragmentation can lead to increased blood pressure, elevated stress hormone levels, and impaired glucose metabolism. All factors that can contribute to pregnancy complications.
On top of that, research has found that pregnant women with OSA have a higher likelihood of requiring a cesarean delivery, experiencing preterm birth, and delivering low-birth-weight infants. Additionally, the disrupted sleep and poor oxygenation caused by OSA can also impact fetal growth and development. So, there’s a chance that the baby may also have health issues both before and after birth.
Why Is Hypertension a Concern for Pregnant Women?
Hypertension, or high blood pressure, is also a health concern during pregnancy. It affects about 10% of all pregnancies worldwide. One of the leading causes of maternal and fetal morbidity and mortality. High blood pressure puts additional strain on the heart and blood vessels. Such strain can lead to severe health complications for both the mother and the baby.
What Are the Types of Hypertension in Pregnancy?
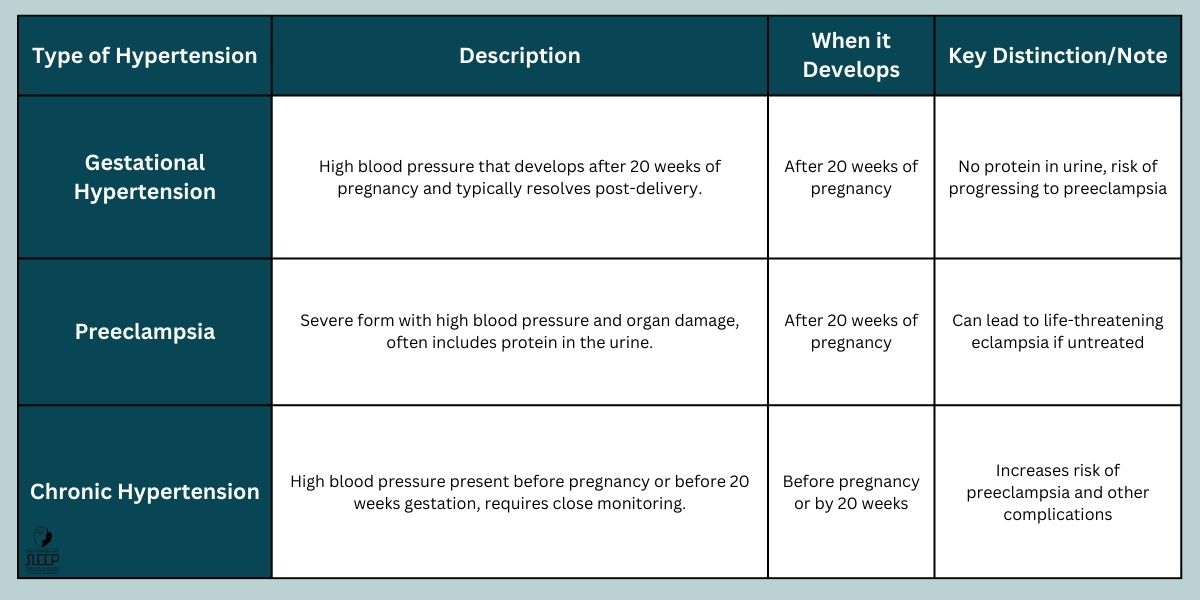
Several types of hypertension can develop during pregnancy:
- Gestational Hypertension: High blood pressure that develops after 20 weeks of pregnancy and typically resolves after delivery. It does not involve protein in the urine, which distinguishes it from preeclampsia. However, women with gestational hypertension are at risk of developing preeclampsia later in pregnancy.
- Preeclampsia: A more severe form of hypertension that usually occurs after 20 weeks of pregnancy. Characterized by high blood pressure and damage to organs like the liver and kidneys. Commonly accompanied by protein in the urine. If left untreated, preeclampsia can lead to serious complications like eclampsia, which involves seizures and can be life-threatening for both mother and baby.
- Chronic Hypertension: High blood pressure that is present before pregnancy or develops before 20 weeks of gestation. This condition requires close monitoring as it can increase the risk of preeclampsia and other pregnancy complications.
Why Is Managing Blood Pressure Important in Pregnancy?
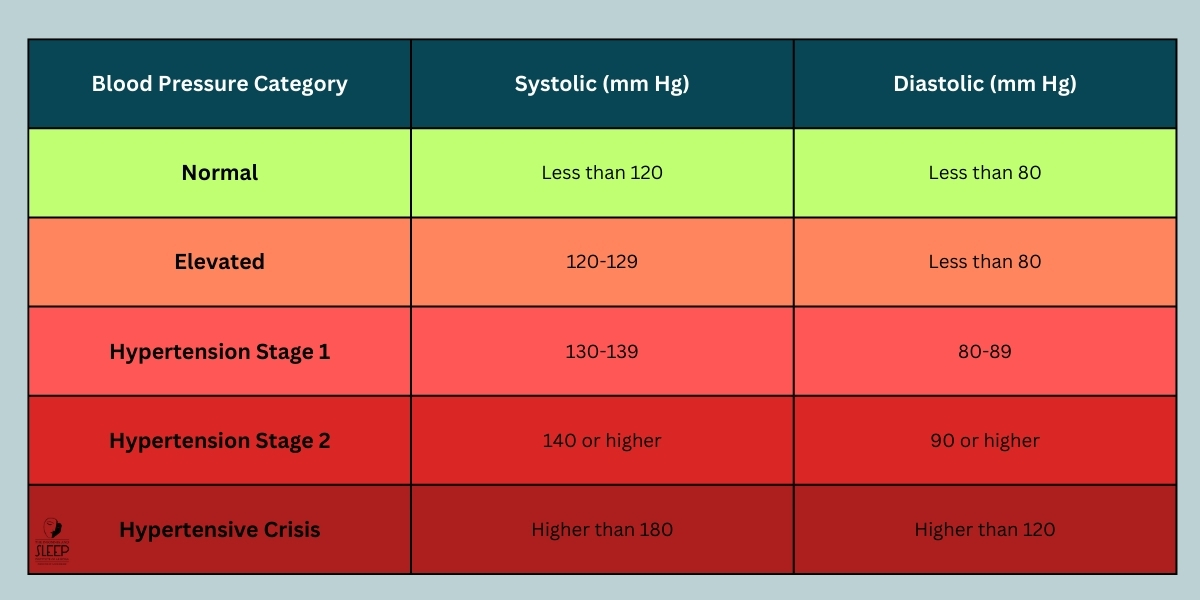
High blood pressure can affect the flow of blood to the placenta. The baby may receive insufficient oxygen and nutrients if the placenta doesn’t receive enough blood. As a result, there is an increased risk of intrauterine growth restriction (IUGR), preterm birth, or low birth weight.
Hypertension is also associated with a higher risk of placental abruption (the premature detachment of the placenta from the uterine wall), preterm delivery, and in some cases, stillbirth. For the mother, uncontrolled blood pressure can lead to heart disease, stroke, kidney damage, and other health problems that may persist even after pregnancy.
What Does the Research Say About CPAP Therapy and Hypertensive Outcomes?
Continuous Positive Airway Pressure (CPAP) therapy is widely recognized as a primary treatment for obstructive sleep apnea (OSA). But what about its role in pregnant women with OSA? Specifically, how does CPAP therapy impact the risk of gestational hypertension and preeclampsia? Recent research answers this important question.
A systematic review and meta-analysis examined six studies involving 809 pregnant women diagnosed with OSA. It provides some compelling answers about the effects of CPAP therapy during pregnancy.
What Does the Study Reveal?
The study aimed to explore the association between CPAP therapy in pregnant women with OSA and the reduction of adverse hypertensive outcomes. The results showed a marked decrease in the risk of developing two critical conditions. Gestational hypertension and preeclampsia.
Key Findings:
- Gestational Hypertension: CPAP use was associated with a 35% reduction in the risk of developing gestational hypertension.
- Preeclampsia: There was also a 30% reduction in the risk of preeclampsia among women who used CPAP.
These findings suggest that CPAP therapy may have a protective effect for pregnant women with OSA, potentially reducing the risk of complications tied to high blood pressure during pregnancy.
How Was the Research Conducted?
This meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. This approach ensured a rigorous and standardized methodology.
Additionally, researchers searched databases such as PubMed, Embase, and the Cochrane Database. They specifically looked for studies examining the effect of CPAP use on hypertension and preeclampsia risks in pregnant women with OSA.
The review focused on data extracted from six original studies. A random-effects model was also used to account for variations between the studies. The analysis provided a pooled risk ratio (RR) to summarize the impact of CPAP therapy on gestational hypertensive outcomes.
What Were the Main Outcomes?
The primary outcomes assessed were the risk ratios (RRs) for gestational hypertension and preeclampsia. The comparison was made between pregnant women with OSA who received CPAP treatment and those who did not.
- Gestational Hypertension: The risk ratio (RR) was 0.65 (95% Confidence Interval [CI], 0.47-0.89; P = .008). This indicates a significant reduction in the risk of gestational hypertension for those using CPAP.
- Preeclampsia: The RR was 0.70 (95% CI, 0.50-0.98; P = .04). A notable reduction in the likelihood of preeclampsia for women undergoing CPAP therapy.
What Is the Significance of These Results?
The study’s results suggest that CPAP therapy may effectively reduce the risk of hypertensive complications in pregnant women with OSA. A notable finding is the reduction in gestational hypertension and preeclampsia. These conditions can lead to serious health issues for both the mother and baby. Potential complications include an increased risk of preterm delivery, low birth weight, and, in severe cases, maternal and fetal mortality.
These findings emphasize the need to recognize and treat OSA during pregnancy. Early intervention with CPAP therapy can help improve pregnancy outcomes. It may stabilize blood pressure levels and reduce the risk of developing hypertensive disorders.
Why Are Age and BMI Not Correlated with the Results?
The researchers also conducted meta-regression analyses to examine whether age or body mass index (BMI) influenced the reduction in risk for gestational hypertension and preeclampsia. The analysis revealed that neither age (coefficient, −0.0190; P = .83) nor BMI (coefficient, −0.0042; P = .87) significantly affected the outcomes.
This suggests that the benefits of CPAP therapy in reducing hypertensive risks apply across various ages and BMI ranges. Whether a pregnant woman with OSA is younger or older, overweight or obese, CPAP therapy may still be effective.
What Should You Do if You Suspect OSA During Pregnancy?
If you suspect obstructive sleep apnea (OSA) during pregnancy, act quickly. Symptoms like loud snoring, gasping for air during sleep, daytime sleepiness, and morning headaches can be warning signs. As stated earlier, OSA can increase the risk of complications like hypertension and preeclampsia, affecting both you and your baby.
First, speak with your healthcare provider. They can evaluate your symptoms and risk factors, such as being overweight or having high blood pressure, and may suggest a sleep study to confirm OSA.
The good news is OSA is manageable. Treatments like CPAP therapy can reduce risks. While lifestyle changes like sleeping on your side and maintaining a healthy weight can improve your sleep health.
Consult with The Insomnia and Sleep Institute of Arizona
If you’re experiencing sleep issues during pregnancy, including signs of OSA, we’re here to support you. At The Insomnia and Sleep Institute of Arizona, our team specializes in diagnosing and treating sleep disorders in both adults and children. We work closely with expecting mothers to provide personalized care and the right solutions for your sleep health.
Using advanced tools like in-home and in-lab sleep studies, we can accurately identify sleep issues like OSA. Once diagnosed, our specialists create treatment plans, including options like CPAP therapy, to reduce pregnancy-related risks and improve your overall sleep quality.
We’re dedicated to offering expert, compassionate care to support your sleep and the health of your growing baby. Don’t let sleep issues disrupt this special time. Reach out to The Insomnia and Sleep Institute of Arizona and let us help you achieve a healthier, restful pregnancy.
References
Dominguez, J. E., Krystal, A. D., & Habib, A. S. (2018). Obstructive Sleep Apnea in Pregnant Women: A Review of Pregnancy Outcomes and an Approach to Management. Anesthesia & Analgesia, 127(5), 1167–1177. https://doi.org/10.1213/ane.0000000000003335
Kanako Bokuda, & Atsuhiro Ichihara. (2023). Preeclampsia up to date—What’s going on? Hypertension Research, 46(8), 1900–1907. https://doi.org/10.1038/s41440-023-01323-w
Lee, Y.-C., Chang, Y.-C., Tseng, L.-W., Lin, W.-N., Lu, C.-T., Lee, L.-A., Fang, T.-J., Cheng, W.-N., & Li, H.-Y. (2024). Continuous Positive Airway Pressure Treatment and Hypertensive Adverse Outcomes in Pregnancy. JAMA Network Open, 7(8), e2427557–e2427557. https://doi.org/10.1001/jamanetworkopen.2024.27557
Xu, T., Feng, Y., Peng, H., Guo, D., & Li, T. (2014). Obstructive Sleep Apnea and the Risk of Perinatal Outcomes: A Meta-Analysis of Cohort Studies. Scientific Reports, 4(1). https://doi.org/10.1038/srep06982