Recently, US News featured a number of factors that worsen sleep apnea—a sleep disorder that circa 24 million adults in the U.S. alone struggle with on a nightly basis. Most have obstructive sleep apnea (OSA), and it’s likely that many more people (children and adults alike) have undiagnosed sleep apnea. It is well established that OSA increased the risk for heart disease, obesity, high blood pressure, stroke, parasomnias, insulin resistance, and memory loss. There is also a link between severe sleep apnea and early death. It is clear that managing sleep apnea is a must and that it is something that requires seeing a sleep specialist.
The Insomnia and Sleep Institute of Arizona is the Face of Sleep Medicine in the area, setting the standard for sleep medicine around the state. As an outcome-driven clinic, every consultation is held with one of our three sleep specialists who can provide a diagnosis to inform testing and treatment. We also offer unparalleled staffing levels with a clinical psychologist, a physician assistant with a Masters in Sleep, teams of experts including respiratory therapists, and nurse practitioners trained in sleep medicine. If you or your child is struggling with any sleep disorder, including sleep apnea, acting fast is a must. CPAP is the gold standard in OSA treatment, but it is also important to address other factors that might be exacerbating sleep apnea.
Are You Worsening Your OSA?
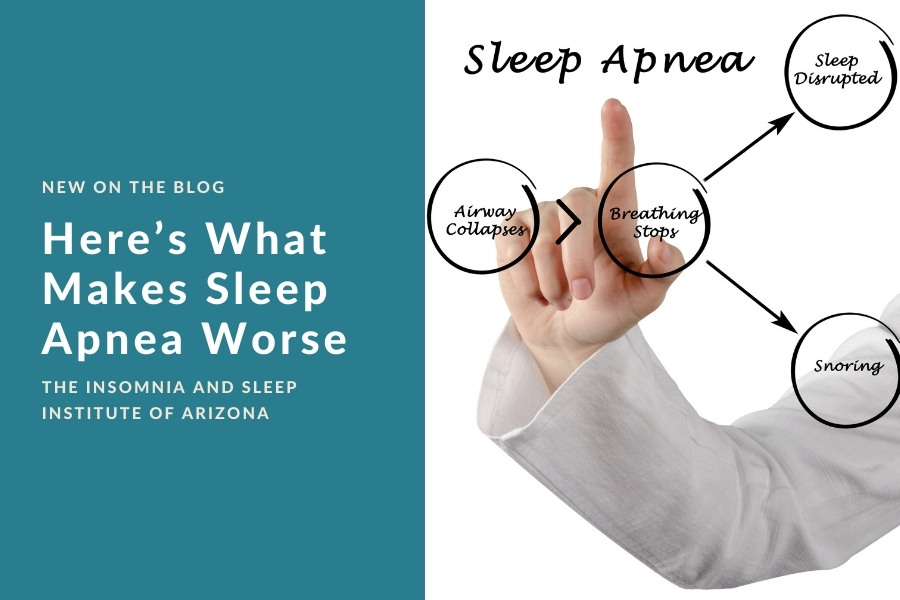
You might not necessarily be “doing” anything to worsen your sleep apnea—it might just be the way you’re made. Anatomy plays a big role in sleep apnea, considering OSA occurs when airflow gets blocked. Throat muscles are supposed to relax when we sleep, but that also makes room for the airway to collapse or for the tongue to get lodged in the way. When this happens, the brain is alerted to the distress, which causes a quick awakening. It’s common for some OSA patients to not remember these frequent wake-ups, but a bedmate might notice snoring, gasping for breath, or snorting at night. In some cases, an anatomic abnormality might be the primary problem, such as a deviated septum, enlarged tonsils, or smaller airway than what is necessary. In these cases, surgery might be helpful, but with most OSA patients it’s not an anatomic problem that’s causing OSA.
An unfortunate new issue with OSA is COVID-19. Those with sleep apnea have been reported to have more severe COVID-19 infections and symptoms, more often transferred to the ICU, and more often need intubation according to a study published in May 2021 in the CHEST journal. COVID leads to a spike in the body’s inflammatory response, and when the body isn’t getting enough oxygen during the sleep hours it triggers an inflammatory response. If you already have lower oxygen levels due to OSA and then you contract COVID, it’s unfortunately natural that you will likely have a more severe infection and symptoms.
You and OSA
Anyone can develop OSA, but a major factor to consider is obesity. Over half of people with OSA are overweight, as reported by the National Heart, Lung, and Blood Institute. Almost two billion people around the world are obese according to the World Health Organization, and one billion people have sleep apnea. When there is excess fat in the neck region, the airway and windpipe are simply more prone to collapse at night. Plus, excess fat on the abdomen can decrease lung volume and make the upper airway more fragile.
In a frustrating chicken or the egg scenario, sleep apnea in itself might also contribute to weight gain. There is even some research that suggests sleep apnea causes a craving for unhealthy foods. One 2019 study in the Sleep journal found that those with severe sleep apnea made poorer food choices than those who had milder sleep apnea. This might be due to the fact that sleep disruption causes the appetite-stimulating hormone in the body to be synthesized and secreted. It also reduces levels of the hormone that suppresses appetite. Additionally, when you’re tired due to poor sleep you don’t have the energy you normally would be active, which can also lead to weight gain.
There are many other factors that are linked to sleep apnea, but the good news is that a sleep specialist can help. If you think you or your child has sleep apnea, schedule a consultation with The Insomnia and Sleep Institute today by calling the office or, for a quicker response, complete the online form now.