Wearing your CPAP every time you sleep is essential for optimal benefits. However, according to a recent study, even using it for a shorter period offers advantages. Obstructive sleep apnea (OSA) is the most common form of sleep apnea. CPAP remains the gold standard for managing OSA. But, alternatives like the Inspire implant are available for rare instances where CPAP fails.
Study Results: Even Modest CPAP Use at Night Reduces Effects of Sleep Apnea
According to research presented by ResMed at the 2022 American Thoracic Society’s annual International Conference stated that “Benefits begin at 2 hours of nightly CPAP use and increase each hour up to 7 hours per night.” The baseline offers a starting point, but using CPAP more extensively yields greater benefits. Researchers evaluated hospitalizations and emergency room visits. The focus is on how nightly CPAP use, from zero to nine hours, influenced health outcomes.
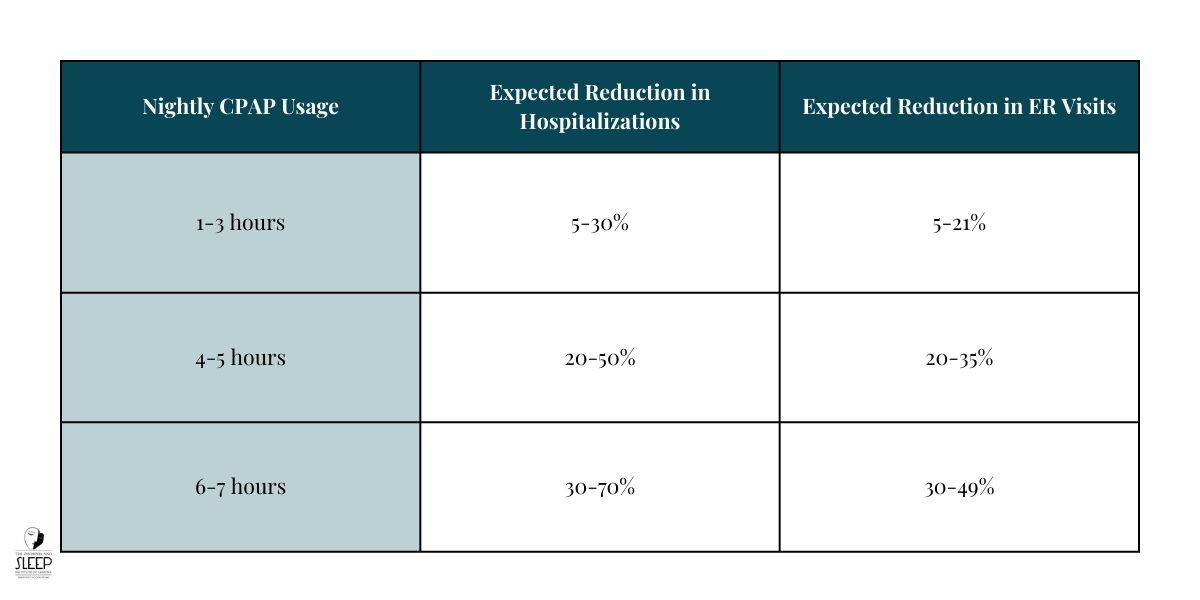
This large-scale study, “Dose-Response Relationship between Obstructive Sleep Apnea Therapy Adherence and Healthcare Utilization,” examined CPAP use in OSA patients. Here’s a concise breakdown of key findings.
Minimum CPAP Hours Needed to Get Health Benefits
- Minimum Usage for Benefits: CPAP therapy for just 1-3 hours per night is enough to yield benefits. It can notably cut down on hospitalizations and ER visits. Such minimal use still brings health improvements. Even a few hours make a difference.
- Dose-Response Relationship: This study discovered a dose-response relationship between CPAP usage and healthcare outcomes. Each additional hour of CPAP use correlated with further reductions in ER visits and hospitalizations. More specifically:
- Hospitalizations decreased by approximately 5-30% with each additional hour of nightly CPAP use.
- ER visits dropped by 5-21% for every extra hour of CPAP usage.
- Sustained Benefits Over Time: Researchers tracked participants for 3, 12, and 24 months. Benefits remained consistent across all intervals. Reductions in hospitalizations and ER visits held steady, showcasing the long-term advantages of even minimal CPAP use.
Study Methodology: Building a Reliable Data Set
The study’s methodology was comprehensive and data-driven, ensuring accurate and meaningful insights:
- Patient Pool: The study analyzed data from 179,188 OSA patients. All were newly diagnosed and started on CPAP therapy (AirSense 10; ResMed) between June 2014 and April 2018.
- Data Sources: Researchers examined data from over 100 U.S. health plans. Linking CPAP usage data let them track patient hospitalizations and ER visits. Monitoring continued for up to two years after therapy began.
- Time Frame for Analysis: Patients’ healthcare resource utilization was monitored over three different time frames—3, 12, and 24 months—to observe how CPAP usage impacted short-term and long-term health outcomes.
Clear Trends in Healthcare Utilization
Even with low usage, there was a noticeable positive impact. Below is a table illustrating these findings.
Why Even Mild CPAP Use at Night Can Deliver Effects
Even brief CPAP use reduces the severity of OSA symptoms enough to lower health risks, especially during critical sleep phases. This partial usage likely prevents the sudden drops in oxygen levels that can lead to cardiovascular strain, one of the primary health risks associated with OSA.
Changing the Way CPAP Usage Is Prescribed for Sleep Apnea
Healthcare professionals may want to rethink how they approach CPAP prescription and compliance. Medicare and Medicaid currently set strict requirements for CPAP use. Patients must use their devices for at least four hours per night on 70% of nights within a 30-day period. If patients miss this threshold, they risk losing insurance coverage for their therapy. Non-compliance could also lead to higher out-of-pocket expenses for patients needing CPAP support.
The lead researcher stresses, “If just two hours of nightly CPAP use can significantly lower a patient’s risk of getting hospitalized, our health systems should encourage and enable people to access and keep using these solutions.” So more flexible standards could lead to better patient outcomes. Such adjustments might reduce barriers to effective CPAP treatment.
CPAP Therapy: Financial Considerations and Coverage for Treatment
Who pays for CPAP therapy is a common concern for many patients. Many are unaware that Medicare, Medicaid, and private insurance plans often cover CPAP therapy.
But there are conditions attached. Adherence must be tracked to ensure that the therapy is being used correctly, as lack of adherence or improper usage are the primary reasons why CPAP therapy “fails” to deliver benefits.

What to Know About Using CPAP for OSA Treatment
CPAP remains the leading treatment for managing OSA. In some cases, it can be combined with lifestyle changes, such as weight loss or a new exercise regimen, to improve results. It works by pushing a steady stream of pressurized air through a mask to keep your airway open while you sleep.
- Immediate Results: Many people feel relief after just one night of use. Better energy. Sharper focus. Fewer morning headaches. It’s a game-changer for day-to-day life.
- Health Booster: Using CPAP can reduce your risk of serious issues like heart attacks, high blood pressure, stroke, and even ease symptoms of depression. Better breathing means better health.
- Compliance Matters: Sticking to CPAP isn’t always easy. Only few users stay consistent long-term, but innovations like softer masks and built-in humidifiers make it more comfortable.
- Customized for You: Machines can be fine-tuned to fit your unique needs. Some even auto-adjusting throughout the night for maximum comfort.
- Portable Options: Compact CPAP machines let you keep up with therapy wherever you go.
At The Insomnia and Sleep Institute of Arizona, we emphasize accurate diagnosis and tailored treatment plans. Millions worldwide are diagnosed with OSA. Many more go undiagnosed or misdiagnosed. This is often due to a lack of self-awareness about symptoms and insufficient screening by general physicians.
No Referral Needed for a Consultation
Scheduling a consultation at The Insomnia and Sleep Institute of Arizona is straightforward. No referral is needed. Our team of sleep specialists is ready to diagnose and treat sleep disorders. To schedule your initial appointment, contact us today by phone during business hours or complete our online contact form for a faster response.
Dr. Ruchir P. Patel Shares His Own Personal CPAP Journey
In this short teaser from the Dr. Ruchir P. Patel: The Real Sleep Doc podcast, Dr. Patel opens up about his own experience with CPAP therapy. Listen to the rest of the episode here.
Stay tuned for more insights in upcoming episodes!





