If you’re one of the millions dealing with obstructive sleep apnea (OSA), you know that quality sleep often hinges on finding a treatment that works for you.
Two leading choices, CPAP and Inspire® implant, offer very different solutions. One involves a mask and a machine. The other relies on an implantable device. Each has unique benefits and challenges. Choosing the right option could mean the difference between tossing and turning—and finally getting the rest you need.
What Is Obstructive Sleep Apnea, and Why Is It Important to Address?
Obstructive Sleep Apnea (OSA) is a sleep disorder that happens when the upper airway becomes blocked repeatedly during sleep, restricting or halting airflow. Each blockage often lasts between 10 and 30 seconds and can occur dozens of times per hour. This interruption forces the body to wake slightly to resume breathing, disrupting normal sleep cycles and preventing deep, restorative sleep.

Key Facts About OSA
- Prevalence: Approximately 936 million adults aged 30 to 69 worldwide have OSA. On top of that, over 425 million cases considered moderate to severe. In the United States, OSA affects nearly 25 million adults.
- Health Risks: Untreated OSA can raise the risk for different health problems:
- Cardiovascular disease: Studies show individuals with OSA have a 2- to 4-fold increased risk of heart attack, stroke, and high blood pressure.
- Diabetes: Approximately 48% of those with type 2 diabetes have OSA.
- Mental health impacts: Chronic sleep deprivation from OSA correlates with an increased risk of depression, anxiety, and cognitive decline.
- Impact on Daily Life: OSA often brings persistent daytime fatigue, making it hard to focus and remember important details. This impacts everything—work performance, relationships, even safety behind the wheel. Studies show OSA sufferers are more likely (2.5 times) to be involved in severe car accidents. Each year, the disorder is linked to thousands of crashes on the road. It’s a serious, often silent threat to everyday life.
Why Is Treatment Important?
Continuous Positive Airway Pressure (CPAP) therapy, the most common treatment, reduces apnea events and improves sleep quality. For individuals who cannot tolerate CPAP, alternative treatments like hypoglossal nerve stimulation (e.g., Inspire® implant) offer viable solutions. Effective treatment reduces cardiovascular strain, enhances mental health, and lowers the risk of motor vehicle accidents.
OSA is a life-impacting condition. Addressing it promptly is important. Not just to improve sleep but to protect overall health and quality of life.
What Are Inspire® Implant and CPAP, and How Do They Work?
Inspire® and CPAP (Continuous Positive Airway Pressure) are two prominent therapies for Obstructive Sleep Apnea (OSA). Each works through distinct mechanisms to maintain airflow during sleep.
CPAP has long been the gold standard for OSA treatment, using a machine to deliver a continuous stream of air through a mask, keeping the airway open and preventing apnea episodes. The continuous airflow acts like an “air splint,” stabilizing the upper airway so it doesn’t collapse. This approach, effective for most OSA patients, reduces apneic events by up to 90% when used consistently.
Inspire®, on the other hand, is a surgically implanted device known as a hypoglossal nerve stimulator. Unlike CPAP, Inspire® doesn’t require an external mask or tubing. Instead, it stimulates the hypoglossal nerve, which controls tongue movement, during sleep. Inspire® gently activates this nerve, moving the tongue forward and lifting the soft palate to keep your airway open naturally. This simple action prevents blockages and supports easy breathing.
Patients turn on Inspire® with a small remote before bed. Then, it works in sync with their breathing patterns throughout the night. Inspire® implant is generally recommended for those with moderate to severe OSA who cannot tolerate CPAP.
Watch: Quick Rundown on Inspire® Implant
Dr. Patel provides a concise overview here.
Dr Ruchir Patel discusses implantable sleep apnea devices on AZ Family News
Pros and Cons of CPAP vs. Inspire® Implant
Here’s a look at the main pros and cons of each treatment option:
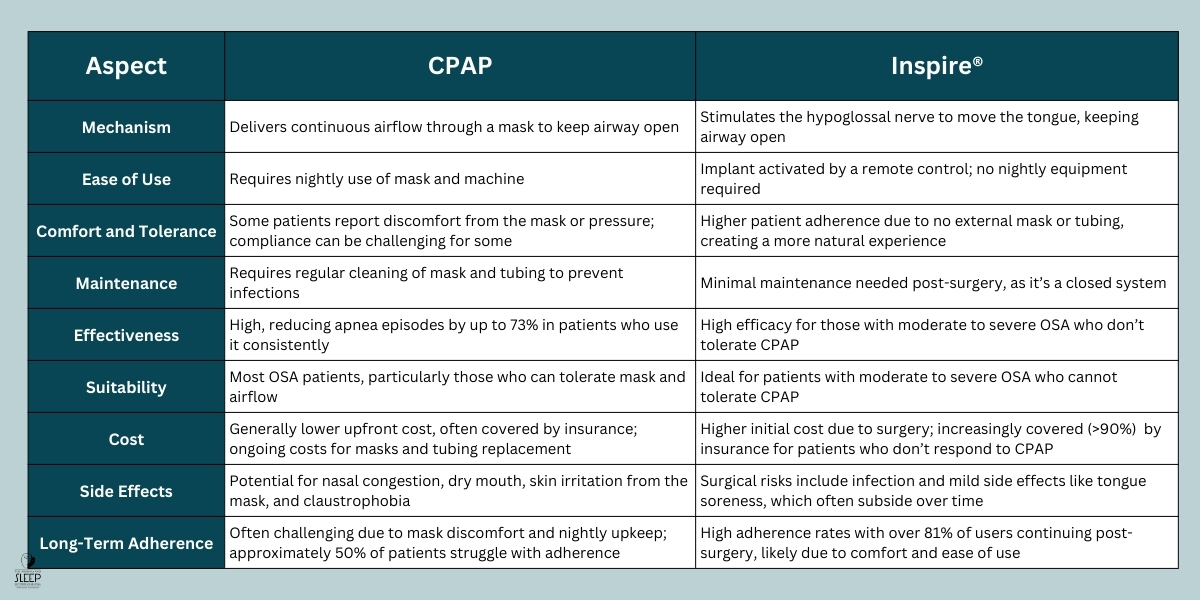
Both treatments bring transformative benefits for those with sleep apnea. But the best choice depends on individual health, tolerance, and lifestyle.
As mentioned, CPAP, known for its effectiveness, is often the first recommendation, especially for new patients. It’s also a more affordable option. However, some people struggle to tolerate regular CPAP use. For them, Inspire® offers an innovative alternative. This option may be ideal for patients who haven’t had success with or can’t tolerate CPAP.
To find the best fit, talk with a sleep specialist who can recommend a solution that feels right for you.
Comparing the Side Effects of CPAP and Inspire® Implant
CPAP (Continuous Positive Airway Pressure) and Inspire® (hypoglossal nerve stimulation) are effective treatments for obstructive sleep apnea, but each comes with potential side effects.
Side Effects of CPAP
- Nasal Congestion and Dry Mouth: CPAP’s continuous airflow can dry out nasal passages, leading to congestion, sore throat, and dry mouth, especially in humid climates or without a humidifier.
- Skin Irritation and Pressure Sores: Prolonged mask use can cause skin irritation, rashes, and pressure sores around the nose and mouth. Studies indicate that up to 50% of CPAP users report skin-related issues.
- Claustrophobia and Discomfort: Some patients feel confined by the mask and experience anxiety, contributing to low adherence. Some patients stop using CPAP within the first few months due to discomfort.
- Ear and Sinus Pressure: Air pressure changes can cause ear discomfort or sinus pressure, disrupting sleep and making CPAP feel less comfortable. These issues can add up, affecting your overall experience with the therapy.
Side Effects of Inspire® Implant
- Surgical Risks: Inspire® requires surgical implantation. Patients may face standard surgical risks like infection, bleeding, and swelling at the implant site.
- Tongue and Throat Discomfort: The device stimulates the hypoglossal nerve, which can cause mild soreness in the tongue and throat. However, most users report these symptoms decrease over time.
- Battery Replacement: Inspire®’s battery requires surgical replacement approximately every 10 years. An additional procedure some patients find inconvenient.
What Does the Research Say About Inspire® Implant vs. CPAP?
Research comparing Inspire hypoglossal nerve stimulation (HNS) and CPAP in treating obstructive sleep apnea (OSA) shows a positive impact on quality of life for Inspire patients, especially for those who cannot tolerate CPAP. In a real-world clinical study, patients with moderate to severe OSA who received Inspire demonstrated significant improvements in quality of life, or “impact on quality of life” (IQoL), over a three-month period compared to those who did not receive the implant.
Key Findings from the Study
- Quality of Life Improvement: The EuroQol utility index, a measure of health-related quality of life, increased significantly in the Inspire group. Scores rose from 0.764 to 0.935 (out of 1.0) in Inspire patients, compared to only a slight decrease in the control group (from 0.733 to 0.727). The positive impact in the Inspire group was estimated at +0.177 (95% CI: 0.044–0.310; p = 0.010), indicating statistically significant improvement.
- Improvements in Key Areas: Patients with Inspire saw particular improvements in everyday activities (p < 0.001) and reductions in anxiety and depression (p < 0.001), showcasing the device’s potential to enhance mental and physical well-being.
- Comparable Quality of Life to the General Population: By the study’s end, the quality of life in Inspire-treated patients was almost identical to that of the general Spanish population of the same age group. The study found no significant difference between the two groups (difference: 0.012; CI95%: −0.03 to −0.057; p = 0.0578).
This research emphasizes Inspire® as a promising option for those who can’t tolerate CPAP. It provides a real boost in quality of life with lasting results. It’s shown to ease anxiety and support higher activity levels. For those seeking a minimally invasive alternative for moderate to severe OSA, Inspire® could be a great fit.
Is the Inspire® System an Option Even if CPAP is Technically Effective?
In most cases, the Inspire® System is considered only if CPAP therapy hasn’t been effective or tolerable, even when CPAP is technically working. Candidates for Inspire® typically need to have moderate to severe obstructive sleep apnea, with a documented inability to sustain CPAP use despite its technical effectiveness.
A recent sleep study confirming this level of apnea is also essential. Moreover, other treatments must have been explored without success. If CPAP is effective and comfortable, Inspire® may not be the best option. This therapy is intended for those who struggle with or don’t benefit from traditional CPAP. It’s designed for when CPAP isn’t the right fit.
A detailed consultation with a sleep specialist will assess your type and severity of apnea and determine the best treatment. Every option aims to improve sleep health. But eligibility depends on your unique needs.
Here’s a video explaining more in depth: Inspire: An Alternative to CPAP Therapy.
How Can The Insomnia and Sleep Institute of Arizona Help You Choose the Right Option?
Finding the right sleep apnea treatment is a team effort. Our specialists focus on your unique needs, taking time to understand your medical history, lifestyle, and comfort with different therapies.
We’re here to help you make an informed choice, whether CPAP, Inspire®, or another treatment is the best fit. You’ll receive guidance and support at every stage. Our team brings experienced care, helping you take steps that lead to healthier, more restful nights.
Explore options that work for you. Schedule a consultation today.
Find expert sleep care at our Scottsdale, Phoenix, and Gilbert locations.
References
Baptista, P., Di Frisco, I. M., Urrestarazu, E., Alcalde, J., Alegre, M., Sanchez, I., O’Connor-Reina, C., & Plaza, G. (2022). Quality of Life Impact of Hypoglossal Nerve Stimulation with Inspire® Device in Patients with Obstructive Sleep Apnea Intolerant to Continuous Positive Airway Pressure Therapy. Life, 12(11), 1737. https://doi.org/10.3390/life12111737
Soundararajan, V., Lor, J., & Fishbein, A. B. (2020). Sleep Apnea and Skin. Current Sleep Medicine Reports, 6(3), 94–100. https://doi.org/10.1007/s40675-020-00179-7
Girouard, A., & Lyda, E. U. (2024, March 19). Inspire Sleep Apnea Device Review 2024. NCOA Adviser. https://www.ncoa.org/adviser/sleep/inspire-sleep-apnea-device-review/
Athanasia Pataka, Seraphim Chrysovalantis Kotoulas, Panagiotis Raphael Gavrilis, Karkala, A., Asterios Tzinas, & Aimiliza Stefanidou. (2023). Adherence to CPAP Treatment: Can Mindfulness Play a Role? Life, 13(2), 296–296. https://doi.org/10.3390/life13020296
Boyd, S. B., Upender, R., Walters, A. S., Goodpaster, R. L., Stanley, J. J., Wang, L., & Chandrasekhar, R. (2016). Effective Apnea-Hypopnea Index (“Effective AHI”): A New Measure of Effectiveness for Positive Airway Pressure Therapy. Sleep, 39(11), 1961–1972. https://doi.org/10.5665/sleep.6224
Bonsignore, M. (2017). Sleep apnea and its role in transportation safety. F1000Research, 6, 2168–2168. https://doi.org/10.12688/f1000research.12599.1
ResMed. (2023, May 8). Sleep Apnea. https://www.resmed.com/en-us/sleep-apnea/sleep-blog/diabetes-and-sleep-apnea/
Kingshott, R. (2014, September 29). Rising prevalence of sleep apnea in U.S. threatens public health – American Academy of Sleep Medicine – Association for Sleep Clinicians and Researchers. American Academy of Sleep Medicine – Association for Sleep Clinicians and Researchers. https://aasm.org/rising-prevalence-of-sleep-apnea-in-u-s-threatens-public-health/
Slowik, J. M., Abdulghani Sankari, & Collen, J. F. (2024, March 21). Obstructive Sleep Apnea. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459252/
Ling, V., Wu, C., & Stiles, S. (2023, October 4). Sleep Apnea Statistics and Facts You Should Know. NCOA Adviser. https://www.ncoa.org/adviser/sleep/sleep-apnea-statistics/